Pancreatic cancer occurs when cells in your pancreas mutate and multiply uncontrollably, forming a tumor. Your pancreas is a vital gland in your abdomen that produces hormones to regulate blood sugar and enzymes to aid digestion. Most pancreatic cancers start in the ducts of the pancreas and are often difficult to detect in their early stages.
Common symptoms include nausea, bloating, fatigue, jaundice, and loss of appetite. Unfortunately, many cases are diagnosed only after the cancer has spread, and pancreatic tumors tend to resist standard therapies.
Despite these challenges, specialized Pancreatic Cancer Treatment in Gachibowli, Hyderabad offers a multidisciplinary approach, including advanced imaging, surgery, chemotherapy, radiation, and targeted therapy - all designed to improve outcomes and provide hope for patients battling this aggressive disease.
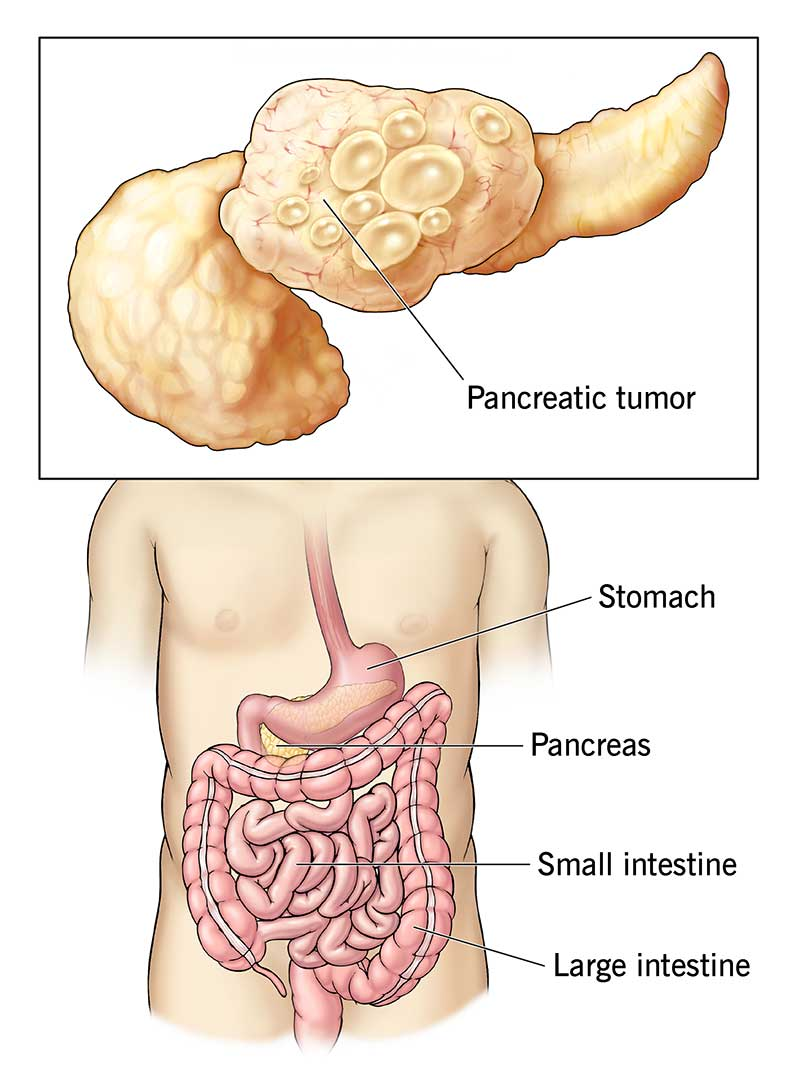
There are two main types of pancreatic tumors:
Pancreatic cancer is responsible for approximately 3% of all cancers in the United States. It’s the 10th most common cancer in men and people assigned male at birth, and the 8th most common cancer in women and people assigned female at birth.
Cases of pancreatic cancer are on the rise. Trends indicate that pancreatic cancer will be the second leading cause of cancer death in the United States by 2030.
Unfortunately, there aren’t any early signs of pancreatic cancer. Symptoms typically emerge once the tumor starts impacting other organs in your digestive system.
Pancreatic cancer symptoms may include:
Your healthcare provider might suspect pancreatic cancer if you’ve recently developed diabetes or pancreatitis — a painful condition due to inflammation in your pancreas.
Symptoms of pancreatic neuroendocrine cancer may be different from traditional pancreatic cancer symptoms, such as jaundice or weight loss. Symptoms can vary, but may include diarrhea and anemia.
There are no tell-tale early signs of pancreatic cancer. Some people develop vague symptoms up to one year before they receive a diagnosis.
Many people report that their first pancreatic cancer symptoms were back pain or stomach pain. These symptoms can come and go at first, but may get worse after meals or when you lie down.
There isn’t a clear answer. We don’t know exactly what causes pancreatic cancer. But experts have identified some risk factors.
A risk factor is something that increases your chances of getting a certain disease. Common pancreatic cancer risk factors include:
Pancreatic cancer tends to spread (metastasize) to nearby blood vessels, lymph nodes, and then to your liver, peritoneum (the lining of your abdominal cavity) and lungs.
The majority of pancreatic cancers have already spread beyond the pancreas at the time of diagnosis.
It’s difficult to detect pancreatic cancer in the early stages. This is because healthcare providers can’t feel your pancreas during routine exams and it’s difficult to see these tumors on routine imaging tests.
If your provider suspects pancreatic cancer, they’ll recommend a combination of pancreas function tests, which may include:
Your healthcare provider may need to take one or more of the following imaging tests:
A pancreas blood test can detect tumor markers. A tumor marker is a substance that may indicate the presence of cancer.
For pancreatic cancer, high levels of carbohydrate antigen (CA) 19-9 — a type of protein released by pancreatic cancer cells — might indicate a tumor.
Sometimes, providers use laparoscopy to determine the extent of pancreatic cancer and whether removal is possible.
During this procedure, a surgeon creates a few small incisions (cuts) in your abdomen and inserts a long tube with a camera on the end. This allows them to see inside your abdomen and look for abnormalities. Often, they’ll take a biopsy during the same procedure.
If you receive a pancreatic cancer diagnosis, you should consider genetic testing. This can tell you if there’s a hereditary reason you developed pancreatic cancer. It can also help your healthcare provider determine which type of treatment will be most effective for you.
Some people with pancreatic cancer have mutations in genes BRCA1 and BRCA2. Though you may recognize these genes as the “breast cancer genes,” mutations in BRCA1 and BRCA2 may also indicate other types of cancer, including prostate, ovarian, and pancreatic.
If you’re a first-degree relative (a parent, child, or sibling) of someone who has pancreatic cancer, you should consider genetic testing. Your results can tell you if you have a BRCA1 or BRCA2 gene mutation. Keep in mind, even if you have the mutation, it doesn’t mean you’ll get cancer. But knowing your risk is important.
Healthcare providers rank pancreatic tumors into four different categories:
If you have specific questions about pancreatic cancer staging, talk to your healthcare provider. Understanding your pancreatic cancer diagnosis can help you make an informed decision about your treatment.
Even though pancreatic cancer has a poor survival rate, complete remission is possible with early detection and treatment. The only way to realistically cure pancreatic cancer is total surgical removal of the cancer.
Specific treatment depends on certain factors, including:
Surgery is the only realistic way to cure pancreatic cancer. But surgeons only recommend it when they think they can remove all of the cancer. Otherwise, there’s little to no benefit.
For surgery to be successful, the cancer must be completely confined to the pancreas. Even then, total cancer removal may not be possible.
There are a few different surgical techniques, depending on the location and size of the tumor:
Chemotherapy uses drugs that kill cancer cells. Healthcare providers give these drugs in pill form or through an IV in your arm.
Providers use chemotherapy as a stand-alone treatment — especially for people with advanced pancreatic cancer. They may also recommend chemotherapy before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
Radiation therapy uses high-energy X-rays to kill cancer cells. Healthcare providers commonly use this approach to treat pancreatic cancer.
Most often, providers combine radiation therapy with chemotherapy (chemoradiation). They may recommend it before surgery, after surgery, or as part of your main cancer treatment. Radiation therapy can also help ease pancreatic cancer symptoms in people who don’t qualify for surgery (in cases of advanced cancer).
This treatment uses drugs that “target” certain proteins. These proteins control how cancer cells grow and spread. Providers may combine targeted therapy with other treatments like radiation therapy.
Common targeted therapy drugs for pancreatic cancer include:
Pancreatic cancer could be very painful as it may involve nearby nerves. Your healthcare provider can help you manage pain with oral medications, anesthesia, or steroid injections.
If you have pancreatic cancer and start to develop severe and persistent pain, tell your healthcare provider. They can find a treatment that will ease your symptoms.
You can’t prevent pancreatic cancer. But there are things you can do to lower your risk:
Healthcare providers don’t usually perform routine screenings for pancreatic cancer. But in people with a high risk of pancreatic cancer due to genetic predisposition, providers recommend monitoring with imaging tests and endoscopic ultrasounds.
If you have a first-degree family member (parents or siblings) with pancreatic cancer, you should talk to a healthcare provider about your risk of developing pancreatic cancer and proper screening and genetic tests.
A pancreatic cancer diagnosis can feel overwhelming. Because everyone is unique, no two cases are the same. Your healthcare provider will assemble a team of experts to determine the best treatment plan for your situation. Your medical team may include:
Generally, it takes about 10 to 20 years for a single cancer cell in your pancreas to turn into a tumor. The goal of ongoing research is to determine how healthcare providers can detect pancreatic cancer in its earliest stages, when it’s more treatable.
In the United States, the five-year survival rate for people with pancreatic cancer is 11%. This means that 11 out of 100 people are still alive five years after their diagnosis.
Survival rates are only estimates. They can’t tell you how long you’ll live or how well you’ll respond to treatment. If you have specific questions about survival rates and what they mean for you, talk to your healthcare provider.
There are no clear-cut symptoms for early-stage pancreatic cancer. However, you should see a healthcare provider right away if you develop:
Develop an open and cooperative relationship with your healthcare provider. If you or a loved one received a pancreatic cancer diagnosis, here are some questions you may want to ask:
As pancreatic cancer progresses, you may develop new symptoms. Advanced pancreatic cancer symptoms may include:
Explore More : Bile Duct Cancer Treatment in Gachibowli, Hyderabad